Across behavioral health and substance use disorder (SUD) treatment facilities, accurate documentation is more than a billing requirement — it is a clinical safety net. Each missed assessment, incomplete treatment plan, or timing error creates both financial and patient risk.
Before Adentris, this Resilient Recovery Treatment, which operates multiple residential programs across Los Angeles, faced the same challenges as many providers: inconsistent documentation across sites, late or incomplete assessments, frequent payor audit flags for missing signatures or outdated treatment plans, and a heavy manual QA workload that could not keep up with daily chart volumes.
The Challenge: Manual QA Couldn’t Scale with Growth
With over 10 beds and dozens of patients a month, the organization relied on 3rd party QA reviews weeks after sessions were closed. Compliance issues often surfaced after billing, making corrections too late to avoid denials or write offs.
Audit sampling showed that 27 percent of progress notes were missing required ASAM criteria fields, 19 percent of treatment plans were not updated every 30 days as required by payors, and one in five discharges were missing physician signatures. These gaps not only threatened reimbursement but also created payors’ audits risk.
The Solution: Real-Time Documentation Assurance Inside Kipu
Adentris integrated directly with Kipu EMR, monitoring every new note, assessment, and treatment plan the moment it was created. Using thousands of behavioral-health-specific quality rules, the platform automatically flagged issues such as missing or outdated assessments (C-SSRS, PHQ-9, CIWA-Ar), mismatched diagnoses and treatment plan objectives, incorrect or missing billing codes for service levels, progress notes lacking time-in/time-out or staff credentials, treatment plans not reviewed within required 30-day intervals, and incomplete discharge summaries or unsigned notes.
Each clinician received instant feedback and could correct issues before submission, creating a continuous documentation process that no longer relied on after-the-fact audits.
What Adentris Found and Fixed
Within the first 60 days, the Adentris platform analyzed more than 5,000 EMR entries and uncovered critical compliance issues in real time., without any manual intervention. These included conflicting sessin times, missing PHQ-9 scores, outdated CIWA-Ar or C-SSRS assessments in 22 percent of charts (for example, a detox patient without an updated CIWA-Ar after Day 3), treatment plan misalignment in 19 percent of charts, incomplete service documentation in 14 percent of charts (such as a group note missing time-out while billed for 90 minutes), expired clinician credentials in 5 percent of records, and billing mismatches in about 9 percent of cases where the documentation supported a lower service level than billed.
All errors were automatically routed to the responsible clinician or compliance lead in real time with built-in coaching prompts that improved both documentation accuracy and clinician understanding.
Results: From Reactive QA to Proactive Excellence
After 120 days of implementation, denials dropped by 62 percent, documentation accuracy rose from 73 percent to 96 percent. Average billing turnaround time decreased by 35 percent, and clinician retraining hours were cut in half. The organization also achieved full audit-ready status for all major payors, including BlueCross, Aetna, and state Medicaid programs.
Beyond Compliance: Elevating Quality of Care
Better documentation led directly to better patient care. The real-time feedback loop helped clinicians identify missed suicide risk reassessments (C-SSRS) within critical windows, catch inconsistent medication notes between nurse and therapist records, and improve continuity of care between residential and outpatient levels. Supervisors reported noticeable improvement in clinical reasoning and treatment plan specificity after several weeks of using Adentris documentation recommendations.
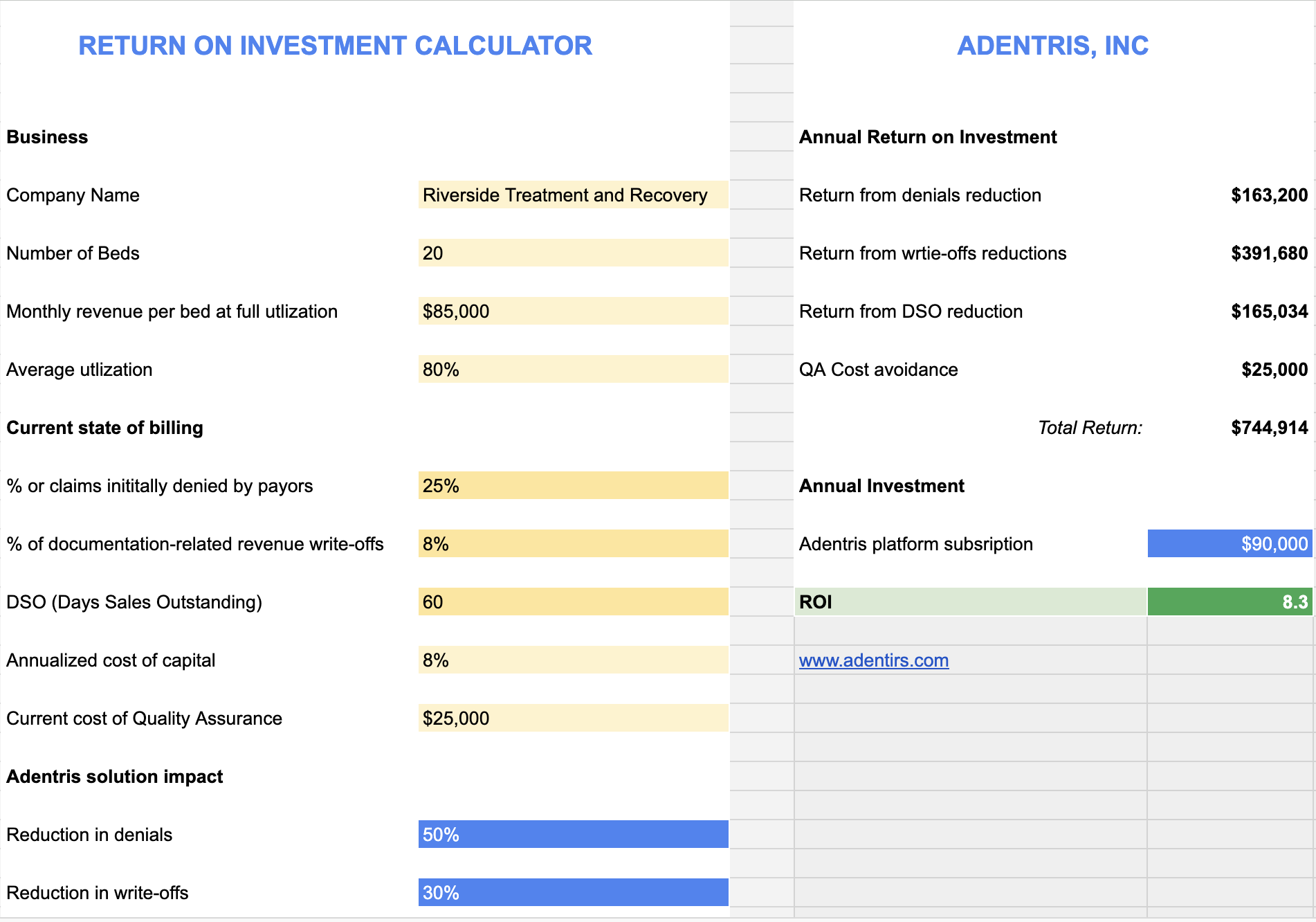
Measurable ROI and Financial Impact
With improved documentation accuracy and faster billing cycles, the organization realized a substantial financial return on its investment. Within the first year, Adentris projects recover an estimated $250,000 in previously lost revenue due to corrected claims based on observed (in 90 days) 62% reduction in denials. Time savings from automation eliminated approximately $5,000 worth spending of manual QA effort a month, worth another $60,000 annually. Denial prevention and accelerated reimbursement improved cash flow by roughly 22 percent, allowing the network to reduce accounts receivable days from 53 to 38.
Overall, the platform implementation for Resilent Recovery Treatment achieved an estimated 7.6x ROI within the first 4 months — combining revenue recovery, labor savings, and reduced compliance risk into a single measurable outcome.
Rebecca L, Chief Operating Officer, Resilent Recovery Treatment:
"Before Adentris, improving documentation quality felt like pushing a boulder uphill. Our team spent hours every week doing manual audits, chasing missing elements, and fixing issues after the fact. It was slow, reactive, and honestly—unsustainable.
With Adentris,everything changed. Our clinicians now get real-time guidance as they document,so issues are corrected before they ever become problems. We’ve eliminated most of the manual review work, raised the overall quality of our charts dramatically,and created a level of consistency we simply couldn’t achieve before. This resulted in our denial rate going down by more than 60%.
I can’t imagine going back to the old way. Adentris made documentation improvement proactive, efficient, and part of daily workflow—not a fire drill.”
Conclusion: A Culture of Continuous Compliance
For SUD facilities, maintaining complete and accurate documentation is not just a financial goal — it is the foundation for safe, consistent, and high-quality care. By embedding Adentris into Kipu EMR, this organization turned every clinician into their own QA partner and every chart into a real-time compliance record.